Did you know the strongest muscles on your body are the the Temporalis, Masseter and Pterygoid? They all work together to move the TMJ (a jaw joint called the Temporomandibular Joint). These muscles are responsible for chewing. And they are the most reliable of muscles on the human body.
However, these muscles can be injured, and healed. Before we discuss this, here’s a quick overview about this miraculous set of muscles.
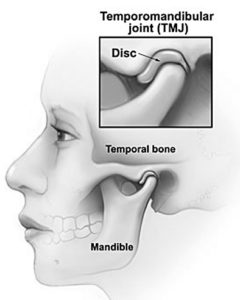
The Muscles of Mastication, more commonly known as the muscles of the jaw, consist of three muscles – the Temporalis, Masseter and Pterygoid Muscles – which work together to move the mandible at the Temporomandibular Joint.
The temporomandibular joint enables your jawbone on either side of your skull. You have one joint on each side of your jaw for mouth movement.
What is a TMJ Disorder?
TMJ disorders — a kind of temporomandibular disorder or TMD — are a group of conditions that affect the Tempromandibular Joint and they can cause pain in your jaw joint and in the muscles that control jaw movement.
The exact cause of a person’s TMJ disorder is often too complex to determine. If you suffer from this kind of pain, it can be from a combination of variables like genetics, arthritis, or jaw injury. Some individuals tend to clench or grind their teeth, which may or may not develop TMJ disorders.
In many cases, the pain and discomfort related to TMJ disorders is temporary. Relieve pain with properly self-managed care. Nonsurgical treatments also can be detailed by your physician. Surgery is likely a final resort well after non-invasive measures have failed.
Signs and symptoms of TMJ disorders are detailed as:
- Painful/tenderness of your jaw
- Pain in either temporomandibular joints
- Aching ear pain inside and/or out
- Difficulty when chewing or pain with chewing
- Pain in facial muscles
- Locking of the joint, making it difficult to open or close your mouth
TMJ disorders can also cause a clicking sound or grating sensation when you open your mouth or chew. But if there’s no pain or limitation of movement associated with jaw clicking, little or no treatment may be necessary.
The time to see a doctor
If persistent pain or tenderness occurs in your jaw, or if opening or closing your jaw completely causes acute pain, a visit to your doctor is most likely your best option. Your doctor, your dentist or a TMJ specialist can detail treatment options at length.
Causes
The temporomandibular joint (TMJ) serves with a hinge action and sliding motions. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which is supposed to maintain smooth movement.
Painful TMJ disorders can occur if:
- There is disk erosion or instability of the joint
- Arthritis aggravates the cartilidge
- Joint damage from blunt trauma
In many cases, however, the cause of TMJ disorders isn’t clear.
Risk factors
Factors that increase the risk of developing TMJ disorders include:
- Numerous types of arthritis like rheumatoid arthritis and osteoarthritis
- Injury to the jaw
- Long-term (chronic) grinding or clenching of teeth
- Certain connective tissue diseases that cause problems which may affect the temporomandibular joint
TMJ and CPAP
Here are some preliminary impressions from various cases of CPAP users.
I am just curious if anyone else has developed TMJ issues while using the CPAP? Being a former mouth breather, I never had any issues until I started using the CPAP. I spent an entire year using chin straps and tape to keep my mouth shut and train myself to breath through my nose. Alan
Nasal masks and pillows can exacerbate TMJ in some patients, but there is lesser a problem with full face masks. The problem lies in the need for nasal mask users to hold their mouths closed against the pressure, and this can cause jaw displacements and grindings. John
I have just woken from my third night with the hose and still feeling the benefits, though the face mask is still not quite right yet. The one big plus is no tension in the head/cranial area this morning as I used my mouth splint. Robert
I have jaw issues (among other things) and once took my mask to my PTist to have her see if the mask’s placement was in any way interfering with anything. Other than having a good giggle at how goofy I looked (I gave her permission to giggle), she said she did not see a problem with the nasal pillows I was using. We went online together and looked at a bunch of the masks. Overall, at the ones at that time, she didn’t think any of them would be an issue. Neither would the CPAP pressure. Paula
I had TMJ surgery back in 1993 (mandibular osteotomy) and prior to the surgery I had daily horrible migraines. I was waking up with horrible headaches again almost a year ago. Also, I was having other symptoms too (shortness of breath/chest pains) but every morning I woke up with a killer headache.
First thing the doctors found out was my oxygen was dropping when I would walk around. Then at my sleep study that found out I was desaturating to 69%. So it wasn’t my TMJ that was causing my headaches this time around it was my oxygen starved brain screaming at me. I wasted a lot of time/delayed treatment blaming it on my good ole TMJ flaring up again.
Not sure if this is happening with you, but you may want to see what your saturations were during your study. Do you think you are clenching/grinding your teeth trying to keep your mouth closed? I worked in dentistry for many years for both oral surgeons and DDS (both clinical and as manager. I can see how those oral appliances they use to treat apnea can mess with a person’s TMJ but I am not sure how a cpap can, unless again, if the cpap is causing you to grind/clench your mouth to keep it closed. Either way discuss it with your doctor and see what he/she has to say. I would be interested to see what they think. Paolo
Assessment and Conclusions
Several points were illustrated above about CPAP and TMJ.
- The stress of keeping the mouth closed when using a nose mask during CPAP may lead to TMJ.
- The use of a mouth device to keep the jaw allignment natural during sleep can lead to grinding or chewing during sleep, thereby leading to TMJ
- Full Face masks can lessen the onset of TMJ or prevent it altogether, presuming a comfortable full face mask is found and used consistently.
- Breathing through the nose for proper PAP therapy regardless of the mask design.
- Post surgery PAP use and long recovery times for the upper airway, especially if sugery was perfomred on the face and the patient has OSA to begin with.
How CPAPClinic can help you, using the above points:
- There are various options for keeping the mouth closed. Try a chin strap and ant-snoring strips.
- An oral device is a very personal investment. We can get you started on this before you visit your dentist.
- When avoiding keeping your mouth closed during therapy, here are some alternative options to consider.
- Post surgical OSA treatment can be difficult but not impossible. Here are some solutions.
Call 1.877.430.2727.
Last Updated: April 6th, 2024
Edited by Bill Bistak B Sc.,SEO/SEM Spc, CRT
Last Updated: March 11th 2024
CPAP Clinic – hеаlthсаrе аt уоur hоmе
We ѕеrvе Grеаtеr Tоrоntо Area іn Cаnаdа.
Cоntасt: 1-877-430-CPAP(2727) or іnfо@CPAPClіnіс.са
Looking tо rent CPAP іn Tоrоntо? Thеn vіѕіt CPAPClіnіс.са аnd сhооѕе from a wide rаngе of CPAP nаѕаl masks in Tоrоntо аnd CPAP nаѕаl ріllоwѕ іn Tоronto

